Scent Habituation and Aromatherapy: Combatting Olfactory Fatigue in Clinical Application
Scent Habituation (also known as Olfactory Fatigue, or “nose blindness”) is the inability to distinguish or “smell” a particular scent as the result of ongoing exposure. The rate at and degree to which humans habituate to scent varies based on the individual as well as the scent itself. While the phenomenon of scent habituation in humans has been studied extensively, the ways in which it impacts the efficacy of aromatherapeutic interventions have been less well analyzed. In this article, we will take a closer look at the mechanisms of olfactory fatigue and its potential impact on the use of aromatherapy, in particular, as it applies to its use in clinical environments.
Scent Habituation: The Science
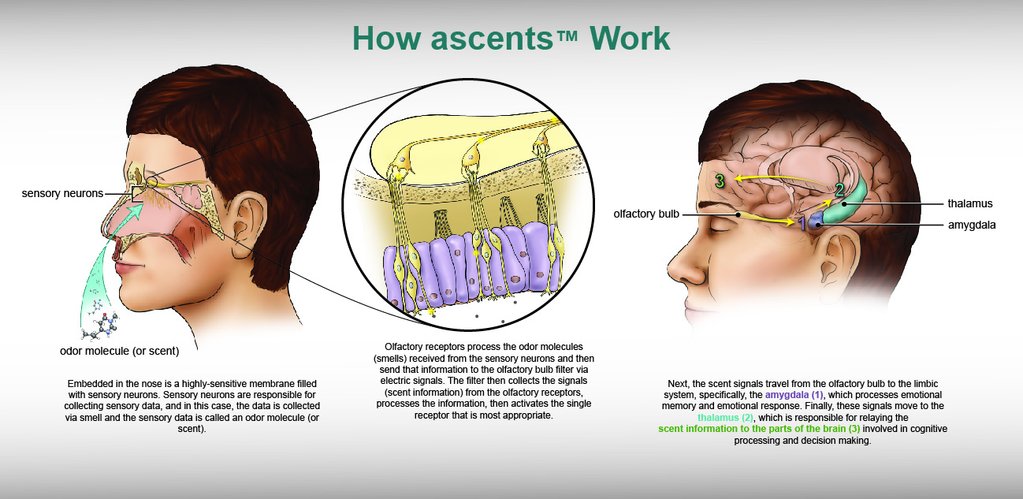
 Habituation, as a general concept, is the brain’s entirely-unconscious way of filtering sensory information. If humans did not habituate to sensory input, our brains would overload and we would be unable to process any new stimuli in our environments, whether sounds, sights or scents — even the potentially dangerous ones. Although all senses are affected by habituation, olfaction, or the sense of smell, is one of the senses most strongly impacted by the phenomenon.
Habituation, as a general concept, is the brain’s entirely-unconscious way of filtering sensory information. If humans did not habituate to sensory input, our brains would overload and we would be unable to process any new stimuli in our environments, whether sounds, sights or scents — even the potentially dangerous ones. Although all senses are affected by habituation, olfaction, or the sense of smell, is one of the senses most strongly impacted by the phenomenon.
Scent habituation is affected by a number of variables, including a given odor’s molecular weight and vapor pressure — factors that a researcher would be hard-pressed to measure without proper equipment. Luckily, there are other elements that are easier to perceive and, therefore, study. A 2017 review of scientific literature published in the journal Physiology and Behavior revealed that olfactory habituation “decreased when odorants had higher intensity…and lower pleasantness. Results suggest that differential habituation to odorants depends on combinations of factors.” [1] Essentially, strong or distasteful scents aren’t as easy to ignore, while pleasant ones will generally lead to faster habituation.
Why Scent Habituation Matters: Aromatherapy in Clinical Environments
Because most aromatherapeutic formulas are pleasant and “light,” they are prone to quick habituation. This means that continual exposure to a scent that should have a positive physiological effect — such as nausea or anxiety relief — will simply stop working once the user’s olfactory receptors have reached a point of saturation.
In other words, if a palliative care patient is exposed continually to an anti-nausea scent formula, while they may initially experience a benefit, that benefit will wear off within minutes if the scent stimulus isn’t removed. Proper application of clinical aromatherapy requires giving the olfactory system the necessary time to “recover” and reset in order for the scent to remain efficacious.
Wearable aromatherapy “patches” or “stickers” that claim to be designed for clinical environments, yet steadily emit fragrance for hours at a time without a chance for olfactory rest, have clearly not taken this into consideration, and are therefore not recommended for clinical application. Aromatherapy is only effective when the scent stimulus remains novel to the olfactory system; continual exposure simply renders the scent ineffectual, usually within minutes.
Combatting Habituation to Aromatherapeutic Scents in Clinical Settings
 There are ways to prevent habituation to therapeutic scents in clinical environments, including post-surgical units, chemotherapy infusion centers, and other like settings. One is by allowing patients to self-administer aromatherapy as needed via an inhaler containing metered doses of essential oil formulas. Single-patient use aromatherapy inhalers can also be administered by nurses and medical assistants as necessary for those patients with very limited mobility. These types of “closed” systems are sanitary and long-lasting, as long as used as directed.
There are ways to prevent habituation to therapeutic scents in clinical environments, including post-surgical units, chemotherapy infusion centers, and other like settings. One is by allowing patients to self-administer aromatherapy as needed via an inhaler containing metered doses of essential oil formulas. Single-patient use aromatherapy inhalers can also be administered by nurses and medical assistants as necessary for those patients with very limited mobility. These types of “closed” systems are sanitary and long-lasting, as long as used as directed.
 Whole-room aromatherapy via ambient diffusion can also be effective in alleviating symptoms such as nausea, anxiety, and pain, especially in settings such as dialysis and chemotherapy infusion centers, but as most whole-room diffusers have only strength settings, this makes habituation a problem in these use cases as well. The only effective way to utilize ambient aromatherapy diffusion effectively is by using a diffuser that includes both a strength and a timing setting, allowing for a proper run/rest scent cycle that gives the patient time to "reset" their olfactory system between exposures.
Whole-room aromatherapy via ambient diffusion can also be effective in alleviating symptoms such as nausea, anxiety, and pain, especially in settings such as dialysis and chemotherapy infusion centers, but as most whole-room diffusers have only strength settings, this makes habituation a problem in these use cases as well. The only effective way to utilize ambient aromatherapy diffusion effectively is by using a diffuser that includes both a strength and a timing setting, allowing for a proper run/rest scent cycle that gives the patient time to "reset" their olfactory system between exposures.
Clinical Aromatherapy Protocols: Critical for Program Success
While the sense of smell (or lack thereof) is highly individual and depends upon a range of variables, what is universal is that all humans experience some degree of scent habituation. This means that aromatherapy programs will be rendered impotent when implemented improperly, i.e. without regard to olfactory fatigue. Designing clinical aromatherapy protocols that reflect this critical facet of olfactory science is ultimately the key to positive outcomes and greater patient satisfaction.
[1] Habituation and adaptation to odors in humans.
Physiol Behav. 2017 Aug 1;177:13–19. doi: 10.1016/j.physbeh.2017.04.006. Epub 2017 Apr 10.
Pellegrino R1, Sinding C2, de Wijk RA3, Hummel T4.